In this section we cover the initiatives and programmes trusts are currently delivering to improve productivity, and highlight the policies and investment required from government and national bodies to help drive up activity levels, eliminate waste, and deliver value for money to the taxpayer.
Initiatives to improve productivity
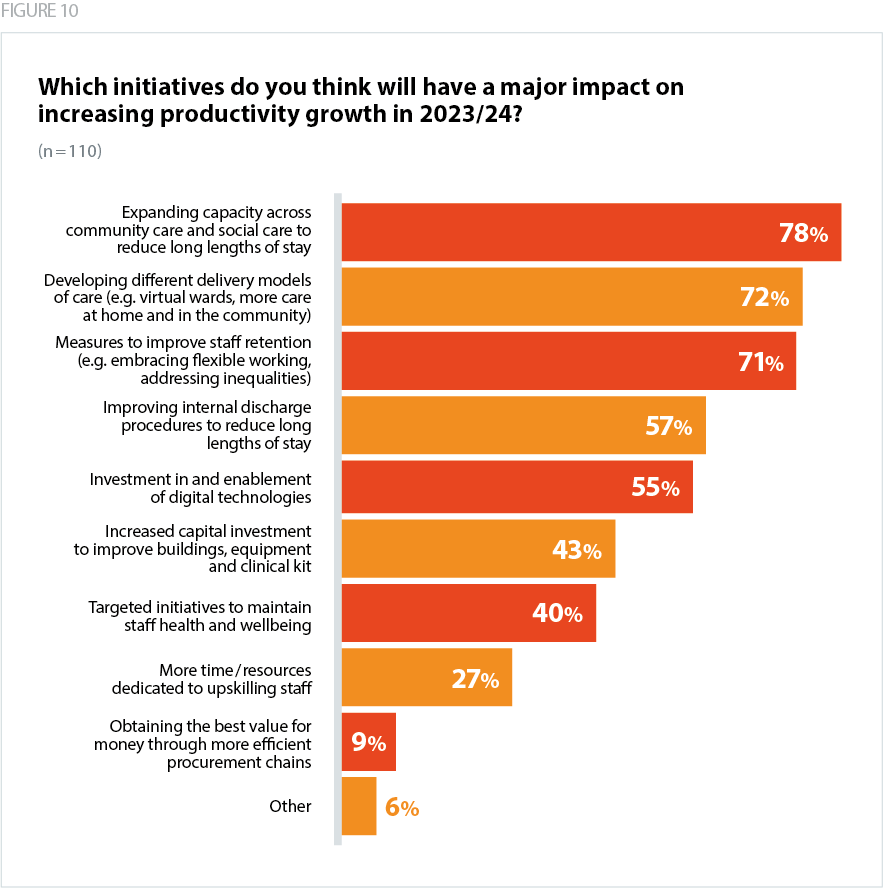
As the graph below shows, trusts have identified a number of initiatives that can help to improve productivity.
Measures to improve staff retention and reduce sickness levels
Staff are clearly impacted by low morale and pressures in the workplace. Targeted initiatives to improve staff health and wellbeing are therefore a key element to improving retention levels. For example, giving staff more meaningful opportunities for flexible working to suit their needs, the chance to take breaks, the ability to rotate between high and low stress settings, and protected time to undertake professional development and to upskill.
However, there is a limit to the effectiveness of these local interventions in the face of stubbornly high vacancy rates. While national and local wellbeing initiatives are usually targeted at improving personal resilience, the resilience of the system as a whole must be assured for them to work. This requires enough staff not only to fill existing vacancies, but to build flexibility into the system.
"Retention, wellbeing and upskilling staff measures will all contribute to improved morale and reduce staff turnover and sickness, avoiding agency, overtime and recruitment and induction costs for new starters." Ambulance trust
Alternative delivery models to improve patient flow and reduce long lengths of stay
Developing different delivery models of care can enable faster discharge by extending care out of acute settings and into the community. This is often better for patients who receive care in the right setting, as well as freeing up hospital capacity for those that need it.
Evidence shows the value and effectiveness of virtual wards in managing risk appropriately in community settings, strengthening intermediate care and reducing the average length of stay of patients in acute settings. As we highlighted in our recent Providers Deliver report, virtual wards were initially used at the onset of the pandemic to ensure as many beds as possible were kept open in acute settings (NHS Providers, 2023b). Since the pandemic, trusts are increasingly working with system partners, including housing and community organisations, and local authorities, to continue to expand support in the community.
Provider collaboratives: improving discharge procedures and joint working
Provider collaboratives are partnerships that bring two or more trusts together to maximise economies of scale and improve care. As we highlighted in our report, Provider Collaboration: realising the benefits of provider collaboratives, they allow trusts to work together to address common problems, such as delivering and consolidating shared clinical support services, and undertaking joint procurement processes (NHS Providers, 2022).
Provider collaboratives can also play a role in delivering material improvements in trusts' internal discharge procedures. For example, some provider collaboratives have implemented single flow management systems, which highlight demand and capacity across the system, and better enable prompt discharges.
In responding to our survey, trust leaders noted the effectiveness of provider collaborative reviews of bed status and flow via engagement with the voluntary and community sectors. Trusts also noted the value of mutual aid – whereby staff are redeployed to other NHS organisations – to meet demand for example for certain referral to treatment (RTT) consultant-led specialties.
Using GIRFT data to inform clinical and operational decision-making
Getting It Right First Time (GIRFT) data is used to improve medical care and deliver efficiencies by reducing unwarranted variation. This data helps identify changes that can be made to care to both improve patient outcomes as well as helping to eliminate inefficiencies.
National GIRFT reviews can inform operational decisions at the trust level, enable comparison of the relative performance of providers, and help material improvements in trusts' productivity. Trust leaders note the value of clinical engagement to develop best practice guidance and identify opportunities for improvement.
While serving as a useful benchmarking tool for clinical staff, it also informs operational decision-making. For example, GIRFT data can provide insights into theatre utilisation and scheduling to help improve productivity across day case work, and help trusts reduce theatre down-time.
"We need the likes of the GIRFT programme to show us where we are inefficient, and we need to have the physical resources available to us – beds and theatres – which are currently being squeezed because of the pressure on the acute care system." Acute trust
Improving coverage and quality of productivity data
Ensuring productivity measures accurately capture trusts’ improvements
There is a concern among a number of acute trusts that estimates about the national productivity gap have been inflated. It is unclear whether the metrics used to capture acute sector productivity, and the extent to which innovations in delivering same day emergency care, are accurately included in national calculations. In addition, trust leaders note the importance of recognising the year-on-year improvement gains made by trusts, rather than focusing exclusively on 2019/20 as the baseline comparator.
Creating a common currency for measuring productivity across all sectors
The Carter Report noted the lack of consistent, quality data and metrics that enabled clear measurements of relative performance (Carter, 2015). The report introduced the 'weighted activity unit' to adjust for differences in case mix between trusts and to provide a common metric to measure hospital output.
There has however been limited national benchmarking for community and mental health trusts' activity and cost base. There is a need to develop a common currency of metrics for community and mental health providers. More work must be done to ensure there are consistent measures of productivity used by the national bodies, trusts and systems.
National discussions about productivity have largely been acute focused. However, as the Hewitt Review notes, to fully capture value across entire patient pathways will require significantly improving the scale and quality of data collection for mental health and community services. The role of mental health and community trusts in improving productivity and supporting the delivery of the government’s recovery plans should be better understood.
Reconfiguring estates to avoid cancellations and increase activity
Trusts are allocating capital funding to reconfigure their estates to reduce their exposure to demand pressures which disrupt planned elective activity. As we highlighted in our recent No more sticking plasters report, separating elective and emergency care supports trusts to cope with Covid-19 waves and seasonal pressures which disrupt planned elective activity. £1.5 billion was apportioned at the October 2021 Spending Review to create surgical hubs and increase bed capacity.
A range of hubs – varying from stand-alone and specialist – can enable surgeons to deliver both low and high-complexity surgery. They provide an opportunity to improve and expand surgical training, ringfence planned treatment, and avoid excessive cancellations due to wider demand pressures.