SUMMARY
The existing NHS model of care is increasingly inappropriate for 21st century health needs. Service transformation to integrate health and care is a potential answer to addressing the complex challenge of rising demand, changing needs, greater efficiency and preventing ill health.
The Five year forward view set out a vision of the NHS moving from fragmented individual institutions to more collaborative, place-based, local health and care systems. Forty-four areas are developing STPs. Trusts have been working hard with key local partners on these plans and are now about to enter important discussions with local communities over the future shape of their services.
Our survey shows that there is growing concern that high expectations around transformation will be undeliverable unless some key barriers and challenges are addressed. While there is strong support for the principles behind the STP process, trust leaders fear the plans are progressing too fast; lack appropriate governance frameworks; and that the public and other key stakeholders such as local councils are insufficiently engaged. They also want more realism about the scale of the challenge and the expected delivery timescales.
Trusts are often at the forefront of driving transformation. For example, providers are leading the creation of a range of new care models, working with local partners to improve care through integration of services around the patient. New models include accountable care organisations; provider chains; and joint ventures between providers to share back offices and provide specialist treatments at scale. Nearly half of the 44 STP plans are co-ordinated by trust leaders. Some areas are making significant progress, often due to strong previous working relationships, with devolution in Manchester being a good example.
The NHS is being asked to deliver a breadth and scale of transformation that many other international health systems have taken at least a decade to achieve. The task is difficult. Providers must manage an increasingly unstable service, deliver transformation and develop complex new local system relationships at a point when leadership and management capacity is already under pressure. Alignment and clarity over local and national objectives are needed, as well as explicit political and regulatory support for innovation and different models. There also needs to be open and realistic acceptance by the national bodies that the required transformation will be stretching, complex and will take time.
THE PROVIDER CHALLENGE
The need for a new model of providing health and care
As the table below sets out, it is increasingly clear that the existing NHS model of service delivery is no longer fit for purpose. The notion that individual institutions will provide highly specialised, inpatient care, focusing on treatment rather than prevention is outmoded.

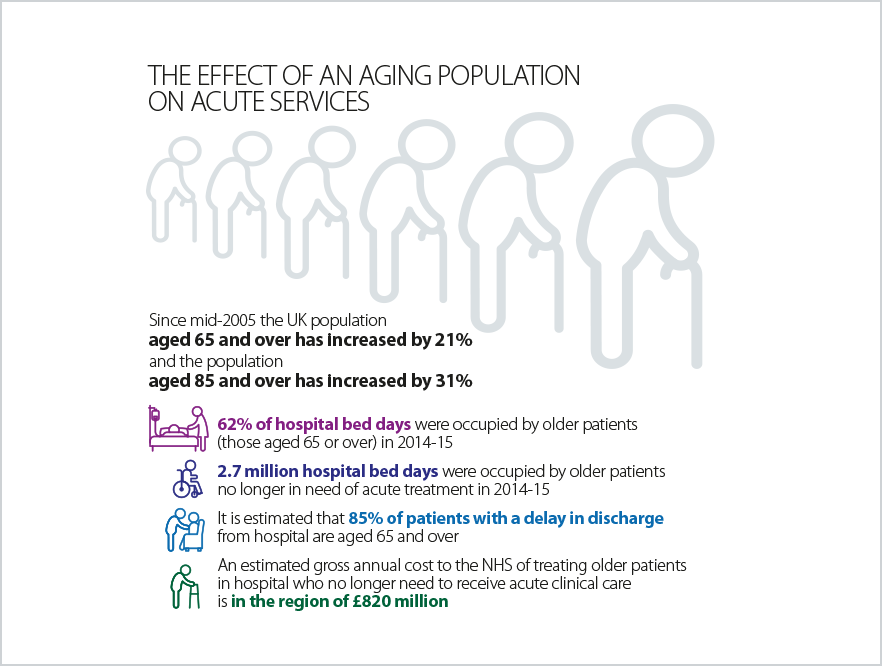
It is difficult to see how the existing NHS model will be able to cope with the significantly increased levels of demand our heath and care system are now facing, as the number of people over 65 rapidly rises over the next few decades. As we show below, the longer people live, the more likely they are to consume health and care services.
No single service, trust or sector can tackle these issues, particularly within the existing NHS model. A new care model based on integration and collaboration is required. Service transformation to integrate patient care is rightly seen as the potential answer to address a number of challenges the NHS faces.
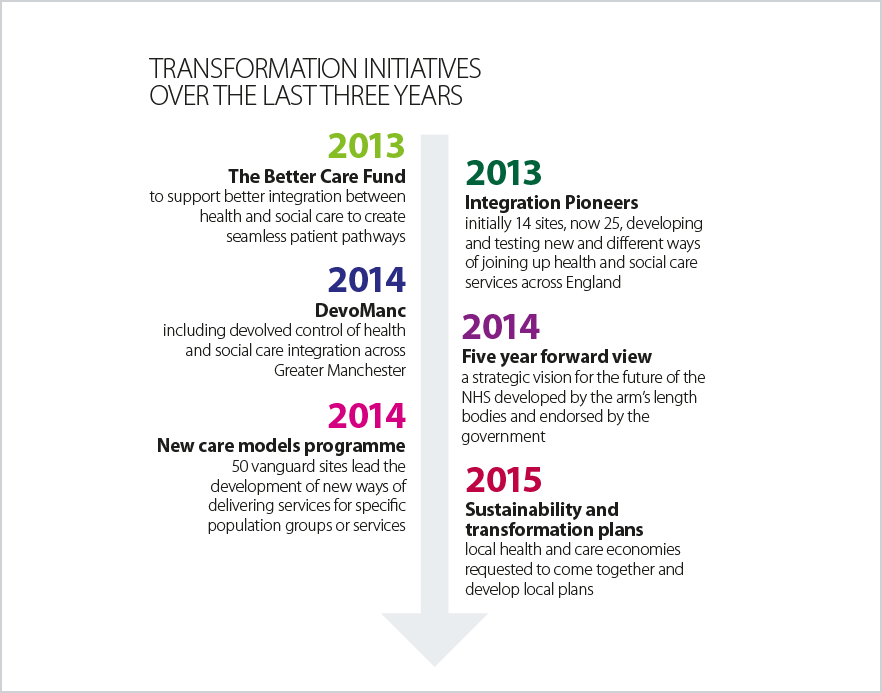
Transformation initiatives
This need for transformation has been widely recognised and, over the past three years, a series of centrally-led approaches have been established to support local transformation, as listed below, with a summary provider view on each.
Barriers to change
Successful implementation of change requires trusts to overcome a number of system and frontline barriers. Quality, governance and operational regulation are still institutionally focused. This misalignment creates a complex scenario in which trusts must balance institutional and STP performance, which can inhibit change. Successful STPs and other forms of system collaboration are dependent on the collective performance of all those in a local footprint. In the words of one trust leader, commenting on the STP process: “The process is entirely reliant on goodwill which is vulnerable to the challenges of demand, acuity and regulation.”
On the frontline trusts are grappling with issues that inhibit more effective day-to-day collaboration: the need for improved and harmonised data systems, streamlined contracting processes, and new governance approaches that reflect the roles and responsibilities of all those involved. One survey respondent commented that there is a “need for a more formal governance framework for decisions underpinned by risk/gain share”.
System overload
Providers report there are four different sources of power and authority in the NHS, each with its own set of priorities:
- NHS Improvement wants providers to achieve financial balance, meet performance targets, maximise their CQC rating, realise efficiency savings and cut agency spending.
- NHS England wants providers to implement the Five year forward view, co-lead their local system towards new care models, help create local system sustainability and transformation plans and implement the outcomes of the cancer and mental health taskforces and the maternity review
- CQC wants providers to deliver the right quality of care and guarantee the right levels of staffing in every setting
- Department of Health wants providers to move to seven-day services, create a paperless NHS, and focus relentlessly on patient safety issues.
Each of these individual priorities on their own are sensible and command provider support. But, taken together, they are far too large a collective set of priorities to deliver consistently and effectively.
THE PROVIDER RESPONSE
Trusts are leading much needed NHS transformation. Often, in a local health and care system, it is providers who can best offer the required management capacity and capability and experience of driving change. Set out below are examples of types of transformation and integration being pursued by providers. They are designed to improve patient experience and better meet patient needs while also improving efficiency. This can be achieved in a number of different ways, including providing more care closer to home or out of hospital; focusing on prevention and greater levels of patient self care; managing demand for hospital services; or better focussing on whole population health.
Accountable care organisations/systems – trusts like Salford NHS Foundation Trust and Northumbria Healthcare NHS Foundation Trust are moving to integrate acute, community, primary and social care with large parts of the commissioning function to create single organisational structures that provide care closer to home more efficiently.
Primary and social care integration – trusts like North, East and West Devon and Royal Wolverhampton NHS Trust are becoming involved in the direct provision of GP services and social care.
Provider chains – trusts like the Royal Free London NHS Foundation Trust, three mental health trusts in the West Midlands led by Birmingham and Solihull Mental Health NHS Foundation Trust and three hospital trusts in Essex led by Basildon and Thurrock University Hospitals NHS Foundation Trust are creating chains of providers with a single shared management team to achieve efficiencies, standardise processes and realise economies of scale.
Joint ventures – trusts are creating joint ventures to deliver treatment across a single pathway. South West London Elective Orthopaedic Care (SWELEOC) has combined the orthopaedic case load of four district general hospitals on a single site, improving outcomes and increasing efficiency.
Specialist franchises – trusts like Moorfields Eye Hospital NHS Foundation Trust are sharing their specialist expertise in the district general hospital setting by running franchises to provide high-quality eye care.
Specialist chains – the specialist orthopaedic hospitals in England are piloting the development of a chain in which they can benchmark outcomes and share expertise.
Integrated services – trusts like Sandwell and West Birmingham Hospitals NHS Foundation Trust, Walsall and Dudley and Walsall Mental Health Partnership NHS Trust, with short patient travel times between them are creating single specialist services covering all three district general hospital trusts in specialties like rheumatology, urology and dermatology.
Trusts are also working hard to develop the underlying enablers to integrate health and social care effectively. These include developing:
- teams with the full range of skills required to assess and meet patient physical, social and mental health needs in an integrated way
- IT applications that integrate GP, community, acute hospital and social care patient data and present it in a single integrated care record
- new ways to contract and manage finances that facilitate and incentivise integrated care such as capitation
- approaches to managing whole population health such as identifying those most at risk of illnesses that are likely to require hospital care and intervening to avoid this.
RISKS
Successful transformation requires some key barriers and challenges to be addressed. The issues that pose the greatest risk are a lack of clear focus, overly ambitious timescales, local engagement and appropriate central support.
Overall there is little confidence among trust leaders that local transformation is happening quickly enough to bring about sustainable integrated patient care and financial balance. As figure 1 below shows, fewer than one in ten trust leaders felt confident of this and 79% were either worried or very worried these priorities would not be delivered.
Figure 4.1
How confident or worried are you that your local area is transforming quickly and effectively to provide sustainable integrated patient car and aggregate financial balance
Lack of clear focus
Central initiatives to support transformation are making some progress. But the number of different approaches, the latest being STPs, and a lack of consistent focus and priorities within these is proving challenging for trusts.
The changing nature of the STP process illustrates this problem. STPs were originally described as ‘the holistic pursuit of the triple aim – better health, transformed quality of care delivery, and sustainable finances’ by bringing all health and care partners around the table to address long-term challenges. Trusts acknowledge the potential of this process. However, they are concerned it has become too focused on issues of immediate financial sustainability as opposed to long-term strategic direction and transformation.
This concern is emphasised by our survey. When respondents were asked to rank the most important aspects of their STPs, ‘returning the health economy to financial balance’ was considered to be the most important issue, with ‘investing in more preventative ways of working’ ranked as lowest in importance.
Figure 4.2
Please rank the importance of the following issues in your STP:
Overly ambitious timescales
There is concern that the STP process, which in many cases relies on creating new, cross local system relationships, is being rushed. And, based on current experience, consistently realising the benefits and improvements from new care models will be a 10-15 year, not a 3-5 year process. National bodies need to accept that the required transformation will take time.
Cultural differences across local health economies means that it takes time to build up the trusting and constructive relationships needed to navigate difficult and sensitive conversations. A key enabler in areas where transformation is most advanced is the longevity and strength of local relationships. One provider leader said: “[we] have been working with CCG/LAs/providers for some years and we already had a strategic vision”. Yet, the timescales attached to both vanguards and STPs are very tight and overly ambitious, as another leader describes: “good progress is being made in collaboration across sectors, but the challenge is significant and the timescale short”.
Lack of engagement at a local level
For transformation to succeed, all stakeholders in each locality must play their part. However, respondents to our survey believe that, in a significant number of areas, there is a lack of engagement in the STP process from primary care and local authorities, as well as local communities. This is worrying considering that local stakeholders and partners will need to be fully engaged if successful outcomes are to be achieved.
Figure 4.3
In your opinion, how engaged are the following stakeholders in the STP process
The role of central support
Effective local collaboration, essential for success, depends on allowing local areas to identify and agree their objectives and action plans. However, as figure 4.3 shows, the majority of chairs and chief executives responding to our survey felt that the STP process has been completely or mostly top down (62 per cent). As figure 4.4 shows, only 7% were also confident that plans and activities from the national NHS leadership are effectively supporting the delivery of a sustainable service in their area.
Figure 4.4
To what extent has your experience been of a national top-down process or a local bottom-up process?
Figure 4.5
How confident or worried are you that plans and activities from the national NHS leadership (the DH and its ALBs) are effectively supporting the delivery of a sustainable service in your area?
As The King’s Fund recently described, some progress has been made by the national bodies to adapt national policy to support the delivery of the Five year forward view and the wider transformation agenda. However, more is needed. Although STPs are progressing at speed, accountability and governance frameworks are lagging behind. In our survey, almost three quarters (73%) of respondents were worried or very worried about this issue and had concerns that STPs have no legal status or authority.
System leaders also must be realistic about the benefits of implementing new care models. The evidence of integration delivering greater efficiencies is weak, relative to the more proven benefits for improving patient experience and some outcomes.
WHAT PROVIDERS NEED
Transformation at the scale required to meet the financial, quality, demand and workforce challenges the NHS is facing will take time, investment and support. It also needs system leaders to support the development of new governance and accountability structures and to ensure that the current, institutionally focused, regulatory structure develops into one focused on local systems.
System leaders need to be realistic about how much can be achieved given the pressure on trust leaders, the current absence of money to invest in transformation and the time it will take to change for the long term.