The last year has seen the NHS begin recovering from the impact of the pandemic, while demand for urgent and emergency care and mental health services hit record peaks. These demand-driven pressures are affecting all NHS services across hospitals, mental health, community, and ambulance sectors. What is more, they are compounded by a persistent workforce shortfall with over 124,000 vacancies in the NHS and more in social care.
The case studies in this report, demonstrate that trusts continue to deliver and innovate within this challenging context. Some of the key themes to emerge include:
Autonomy and leadership
Approaches to leadership that promoted the autonomy of clinical staff, while protecting them from some of the bureaucratic burden that can slow down patient flow, was a recurrent theme.
The value of collaboration
No single organisation can resolve these long-standing, systemic issues on their own. Trust leaders understand that working collaboratively across systems with other providers and partners, including primary care and social care, using existing capacity effectively, focusing on prevention and effective demand management, are key to improving patient flow.
A focus on admission avoidance
Delivering more out-of-hospital procedures or using an ambulatory care pathway has proven to be an effective way of reducing unnecessary admissions, offering the same standard of treatment more efficiently for patients while freeing up inpatient capacity.
Prioritising care at home and intermediate care
Virtual wards and remote monitoring of patients has proven to be an effective way of moving more care into community settings, reducing average length of stay, supporting intermediate care and rehabilitation, and improving people’s experiences of care.
Similarly, building outpatient capacity, including developing the community workforce, can see more complex care including mental health care delivered outside of traditional hospital settings, allowing people to remain more independent, or close to family, in familiar surroundings at home while accessing the support they require.
The importance of population health approaches
The core purpose of the health service is to improve health as well as treating illness. Trusts able to use population health approaches to design services around the specific needs and demands of the communities they serve, are seeing the benefits. Trusts reported real value in the effective use of analytical methods to identify and predict demand, working with partners on preventative initiatives to support patients before they reached crisis.
A long road ahead
NHS England’s two-year urgent and emergency care recovery plan sets out a range of headline targets for both ambulance response and A&E waiting times to ensure a swift response for patients most at risk. Importantly, the plan also recognises the solutions for tackling long waits for urgent and emergency care must involve system partners and also include a focus on the development of pathways for patients who do not require an ambulance response or hospital care.
Achieving a lasting and sustainable recovery will take years, but it will also require collaboration and action across the entire provider sector and with integrated care system (ICS) colleagues. Trust leaders are keenly aware of this, as demonstrated in these case studies. However, in the medium to long term, national action to ensure better workforce planning, capital investment and expanded capacity remain key to success.
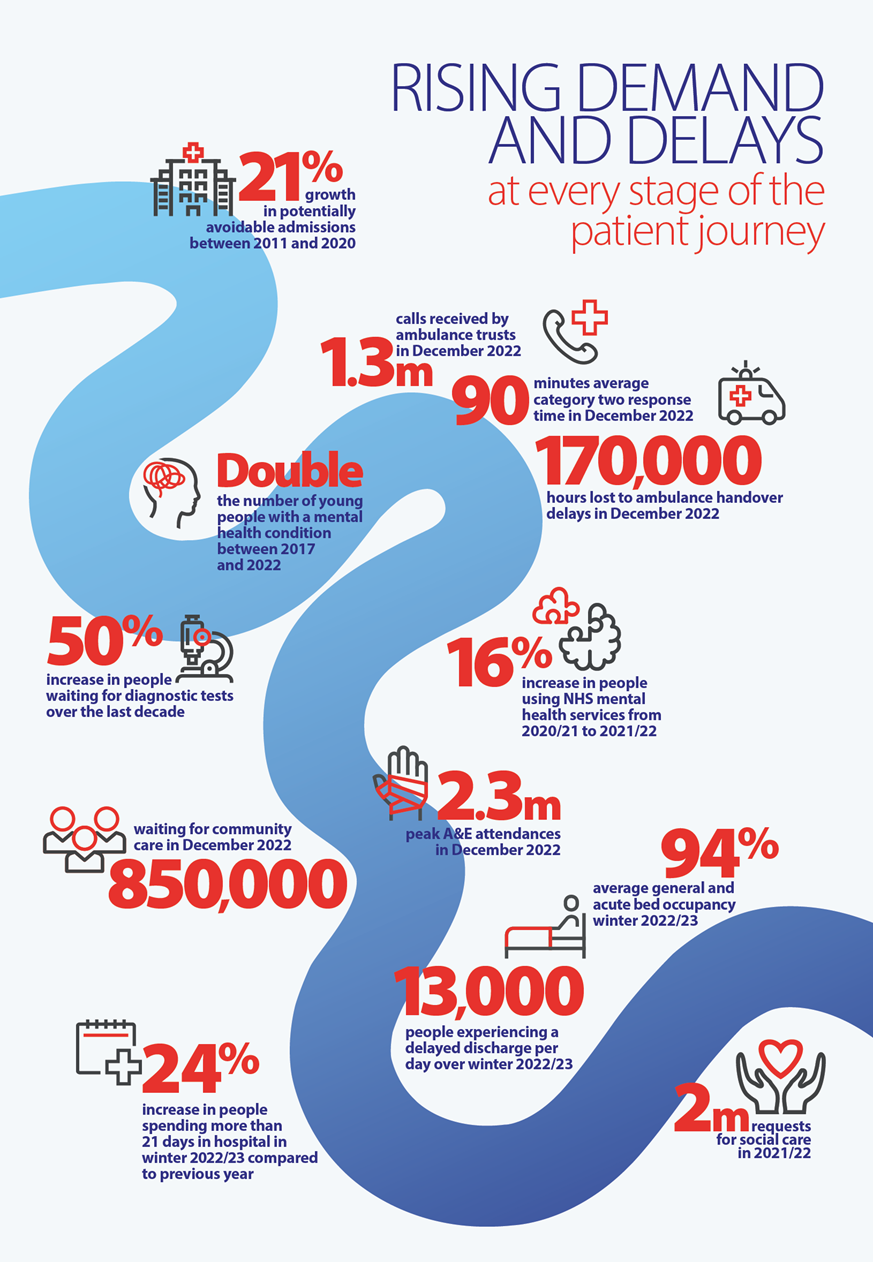
The infographic below shows key pressures and pinch points charting patient journeys across the health and care system.
Sources for infographic
21% growth in potentially avoidable admissions between 2011 and 2020, Nuffield Trust analysis of HES data
1.3 million calls received by ambulance trusts in December 2022, NHS England
90 minutes – average category two response time in December 2022, NHS England
170,000 hours lost to ambulance handover delays in December 2022, NHS England
Double the number of young people with a mental health condition between 2017 and 2022, National Audit Office
50% increase in people waiting for diagnostic tests over the last decade, NHS England
16% increase in people using NHS mental health services from 2020/21 to 2021/22, NHS Digital
2.3 million – peak A&E attendances in December 2022, NHS England
850,000 waiting for community care in December 2022, NHS England
94% – average general and acute bed occupancy winter 2022/23, NHS England
13,000 people experiencing a delayed discharge per day over winter 2022/23, NHS England
24% increase in people spending more than 21 days in hospital in winter 2022/23 compared to previous year, NHS England
2 million – requests for social care in 2021/22, NHS Digital