

This weeks’ data release was a double whammy – week 6 of the winter weekly sitreps and NHS England’s monthly performance data for November/December 2017, plus the latest flu report from Public Health England. The data confirms what many are saying on the frontline, that pressures this winter are severe and that demand for services continues to rise inexorably. Despite the heroic efforts from staff we have been highlighting, the key standards are now simply undeliverable as we have argued in our letter today to the Secretary of State for health and social care.
The highs
Despite the headlines, we must not lose sight of some of the positives from today’s data. NHS trusts have been working hard to manage increasing demand; maximising the efficiency of the available resources and improving patient care.
- The focus since the start of the financial year on delayed transfers of care has seen a significant reduction and this continued in November 2017; with the average number of delayed beds 5.8% lower than the previous month and 19.8% lower than November 2016.
- Performance against the key cancer targets has been relatively stable over the past few months. And while the 62-day wait from GP urgent referral to first treatment target is still being consistently missed, in September to November 2017 performance was better than for the same three months the year before.
- In November 2017 89.5% of patients were waiting 18 weeks or less for elective care, one percentage point lower than the same month the year before. However in the last 12 months 16 million patients started treatment, 4.5% more than the previous year.
- Compared to the last week of December this weeks’ sitrep shows acute trusts have opened up around 2,000 additional escalation (temporary) beds to provide extra capacity.
- By the end of November 2017 59.3% of frontline healthcare workers had been vaccinated against flu, up from 55.6% the year before.
The lows
The December performance data and the weekly sitrep, covering 1-7 January, make for starker reading; with the full impact of winter pressures starting to bite.
- A&E performance in December 2017 was record breaking, but sadly for the wrong reasons. The month saw both the highest ever number of emergency admissions – over 520,000 – and the lowest ever performance against the 4-hour standard for type 1 (major) attendances – 77.3%.
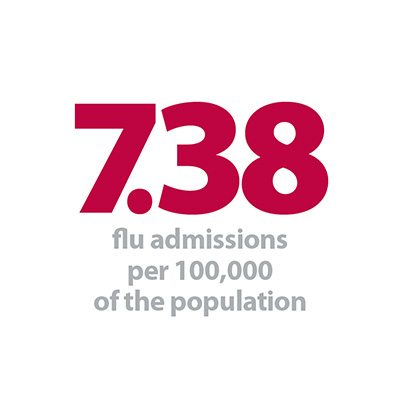
- This increase in admissions is compounded by the rising number of flu cases, with 7.38 hospitalised cases of influenza per 100,000 of the population this week, up from 1.55 two weeks ago. Of the 758 hospitalizations, 240 were admitted to intensive level care.
- More admissions means more beds are required. But despite the extra capacity bed occupancy levels have increased, peaking at 95.8% on 3 January with 88% of hospitals reporting occupancy of over 92% that day, the level above which NHS Improvement recommends escalation processes should be implemented.
- High bed occupancy has a significant impact on flow through the hospital, reaching right back to the front door. This week’s sitreps also showed the worst performance so far this winter for ambulance handover delays, with 1 in 6 delayed by 30 minutes or more and 1 in 20 delayed by over an hour.
We asked one of our members, Kate Slemeck, chief operating officer at Royal Free London NHS Foundation Trust, what this demand feels like at the frontline:
"The new calendar year has started with high numbers of ambulances arriving at our emergency departments at Barnet Hospital and the Royal Free Hospital, with patients who are genuinely sick and in need of hospital services. Acuity is acknowledged to be high by hospitals and ambulance services alike. We are also seeing patients admitted with influenza, a number requiring intensive care level support."
We are working closely with our local healthcare partners – other hospitals, CCGs and local authorities – to coordinate care and act responsively, and to ensure we deliver the very best care for patients given the demand and resources available.
Chief Operating Officer, Royal Free London NHS Foundation Trust
"We have been extensively planning in advance of winter to ensure we can continue to deliver safe care; including significantly reducing our elective programme, and rescheduling outpatient clinics to free up medical and nursing staff to support the increased demand for emergency services.
We have also received funding which has meant we have been able to provide additional capacity to help meet this demand (this being agreed in late December). In addition we have run the SAFER Start programme on both our acute sites – this is a multi-agency approach to supporting patients to be discharged from hospital as quickly as possible. As part of this, all non-essential meetings are cancelled to allow non clinical staff to support their colleagues on the wards.
We are working closely with our local healthcare partners – other hospitals, CCGs and local authorities – to coordinate care and act responsively, and to ensure we deliver the very best care for patients given the demand and resources available.”
Responding to today’s figures, NHS Providers director of policy and strategy, Saffron Cordery, said:
"These figures reflect the exceptional challenges we are seeing this winter. We have more patients coming in, and many of them are seriously ill, and that is why we are seeing emergency admissions at record levels.
"The NHS put in place extensive preparations for winter, but despite opening nearly 2000 additional beds last week to cope with the additional pressures, bed occupancy was at 95 per cent, well above the recommended safe limit of 85 per cent.
As we have outlined in our letter to Jeremy Hunt, it is time for the government to address the long term funding of health and social care, and make the big decisions needed no later than the autumn Budget, to ensure the health service can meet the standards of care enshrined in the NHS constitution.
Director of policy and strategy, NHS Providers
"It is also worrying that last week we saw an increase in delays of more than an hour for patients being handed over from their ambulance to A&E. That is a sure sign of difficulties coping with the number of patients who need to be admitted, and by taking ambulances off the road it also raises the risk of delays for other people who call for help.
"The truth is that the NHS can only do so much with current funding. We have reached a watershed moment. As we have outlined in our letter to Jeremy Hunt, it is time for the government to address the long term funding of health and social care, and make the big decisions needed no later than the autumn Budget, to ensure the health service can meet the standards of care enshrined in the NHS constitution.
"Failure to act now will lead to those standards moving further beyond reach. This would harm the quality of care, causing delays and distress for patients and weakening staff morale. It could also undermine public faith in the NHS.”