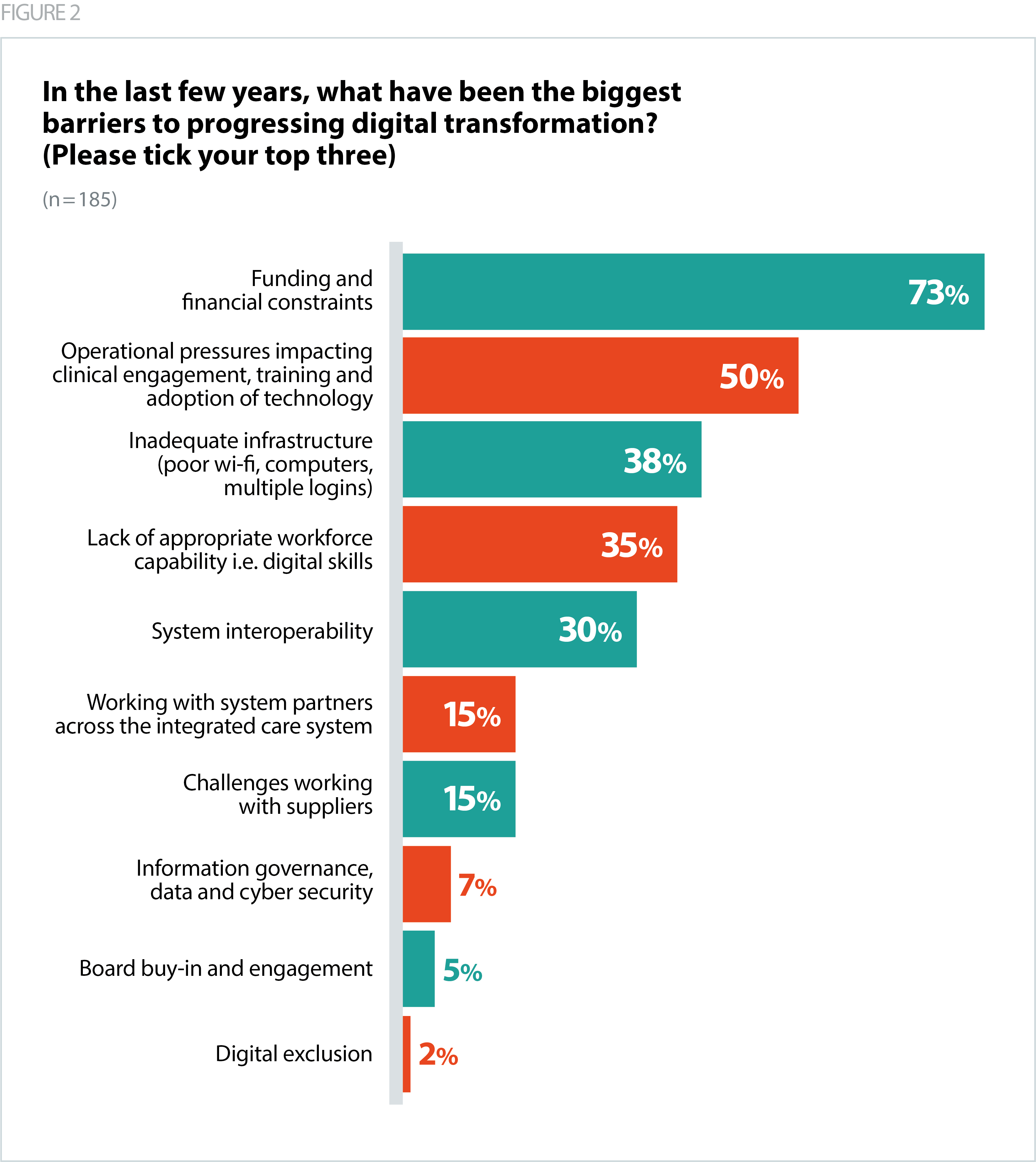
Barriers to progressing digital transformation
Despite the key role digital plays in ensuring a 'next generation' NHS, trusts are not yet able to fully leverage the potential of digital.
The will to change is absolutely there, but digital is still seen as a separate thing to core business and therefore it is in the difficult space of no capital to grow, reduced revenue to support expert people (who can be hard to come by anyway) and escalating ambition.
Funding and financial constraints
Financial constraints are impacting on trusts' ability to push forward the digital transformation agenda for several reasons.
In this survey, trust leaders reflected that a lack of funding has impacted the ability to implement or upgrade critical systems like Electronic Patient Records (EPRs). The way in which digital is funded is also creating a barrier for trusts. There is an urgent need for access to capital as well as increasing need for revenue to enable digital transformation. Trust leaders also reflected that small, late-in-the-year funding allocations are unhelpful. In order to plan strategically and make efficient use of resource, trusts need larger multi-year funding that can be used with discretion to meet local needs including sustainable funding for digital teams.
These barriers aren't new for trust leaders, and many have been grappling with this challenge for several years. The 2023 State of the Provider Sector survey conducted by NHS Providers also evidenced trusts' feelings of insufficient levels of investment for digital transformation. Just under two thirds (63%) of trust leaders strongly disagreed (33%) or disagreed (30%) that their trust will have access to sufficient capital funding to transform and continue the journey to digital maturity, and 60% feel the same about capital investment in business-critical IT infrastructure or systems.
The top issue is the piecemeal uncertain nature of digital funding and its massive impact on delivery. We can't develop multi-year plans. We have to get small pots of money and hope we can knit them back into a coherent digital solution.
Finances are the biggest barrier. We may receive the 'nod' to progress many digital activities, but without funding streams they grind to a halt. And even when national money is made available, there are many restrictions for using the money and tight timescales, which make it impossible at times.
Operational pressures impacting clinical engagement, training and adoption of technology
The survey findings underscore that relentless operational pressure on NHS staff contributes to a lack of workforce capacity to engage with digital programmes. This has also left trust leaders and staff with limited headroom for undertaking large scale digital transformation programmes that could see the greatest long-term benefit to staff and patients. Trust leaders also reflected that staff capability to adopt new technology and ways of working impacts the adoption of technology and hampers the pace of change in many trusts.
Having a mobile workforce makes education and training more difficult, including abstractions from duty to undertake training, comes at the expense of operational performance.
Lack of workforce capability
Recruiting and retaining digital skillsets and developing digital capabilities within the workforce are critical for successful adoption and utilisation of technology. This includes supporting the development of Digital, Data and Technology (DDaT) skillsets, for example, by building expertise across user centred design, user research, clinical, operational and analytic skillsets. Survey respondents also highlighted the importance of clinical engagement, user centred design and appropriately resourced implementation of technologies, including staff training in assuring the effectiveness of digital tools and systems.
In this survey, trust leaders reflected that the ability to recruit these skillsets is severely impacted when competing with private sector markets. As trusts look to innovative tools such as artificial intelligence (AI) or to bolstering their cyber readiness, they will need to develop their capability and capacity to deliver.
The ability to recruit sufficient substantive staff into the organisation is severely hampered by the poor rates of pay offered compared to the private sector. The consequence of sizeable vacancies for difficult to fill roles is a major barrier.
System interoperability
The ability of technical systems, organisations, and people to exchange and make use of information is one of the biggest technology challenges for the health and care system. The landscape is complex as different parts of the health and care system have varied ways of working and use different ways of communicating. There is a need for national support to tackle the interoperability challenges that are faced throughout the NHS, including around supplier management and setting standards.
National clinical system providers are not responsive to individual trusts/integrated care systems. National action is required to hold them to account for delivering interoperability and real time data.
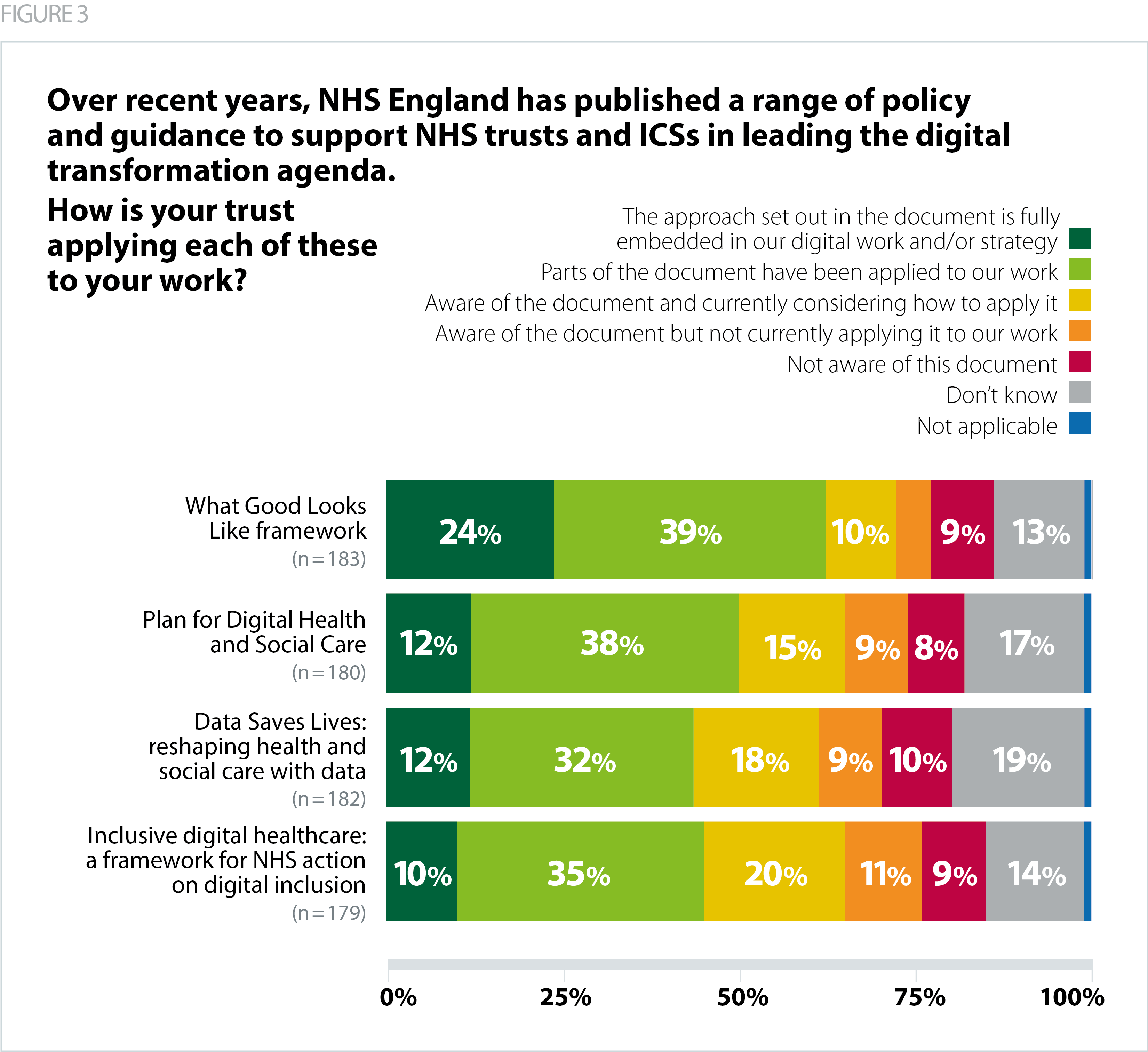
National direction and policy
Trust leaders are engaging with national support, frameworks and programmes, in particular embracing the What good looks like framework for digital transformation, but would welcome further clarity on the national direction of travel and look forward to the ten year health plan providing that vision.
In this survey we asked trust leaders whether they were utilising national guidance from NHS England (NHSE). Respondents were most likely to have the approach set out in the What good looks like framework fully or partially (24% and 39%) embedded in their digital work and/ or strategy compared to NHSE's other policy and guidance documents. [see Figure 3.]
Over half (54%) of trust leaders said they were very confident (22%) or confident (32%) their trust will meet the minimum digital standards by 2025, set out in a Plan for digital health and social care, including the need for all providers to implement an EPR. 8% of respondents said their trust had already met the target.
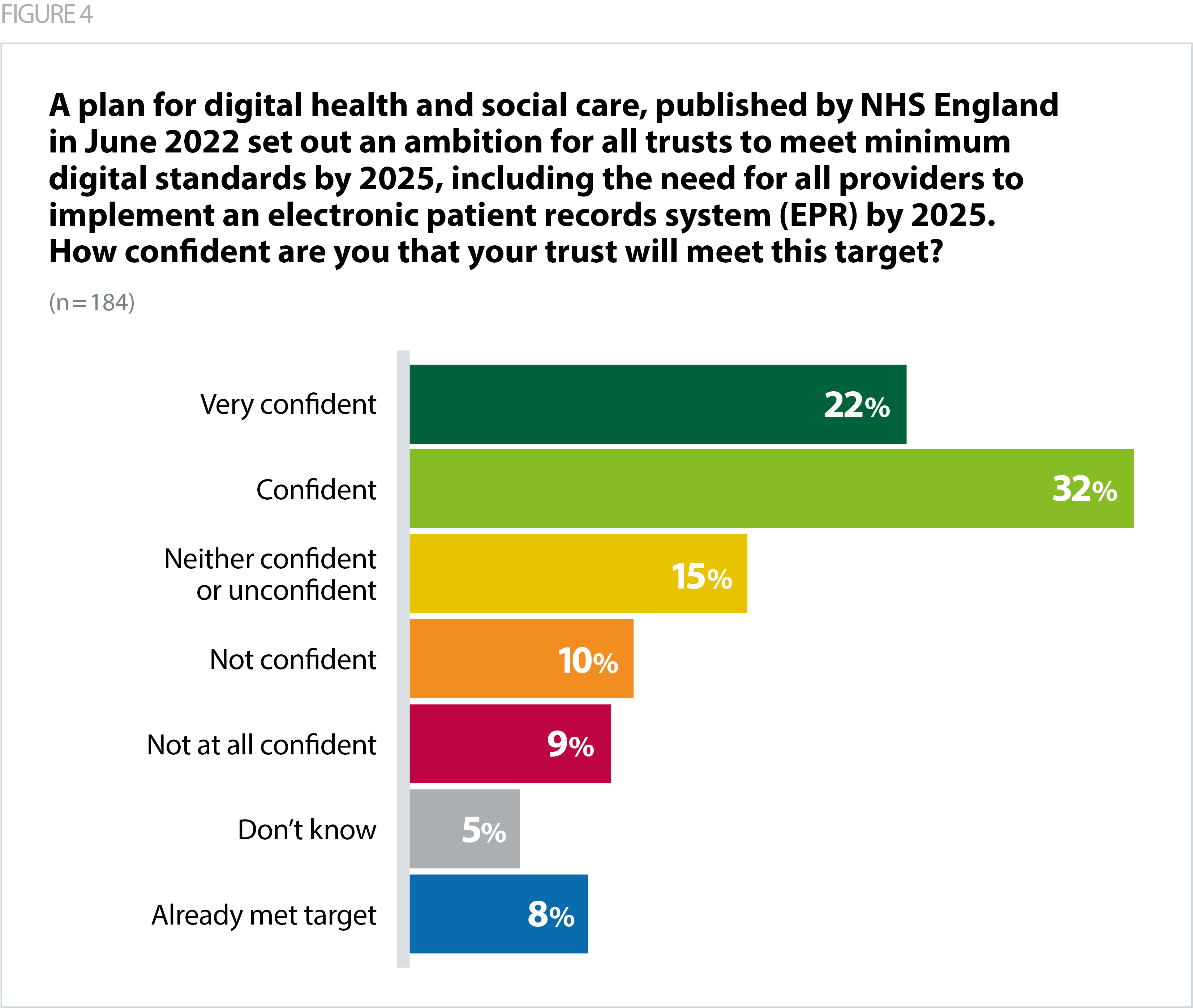
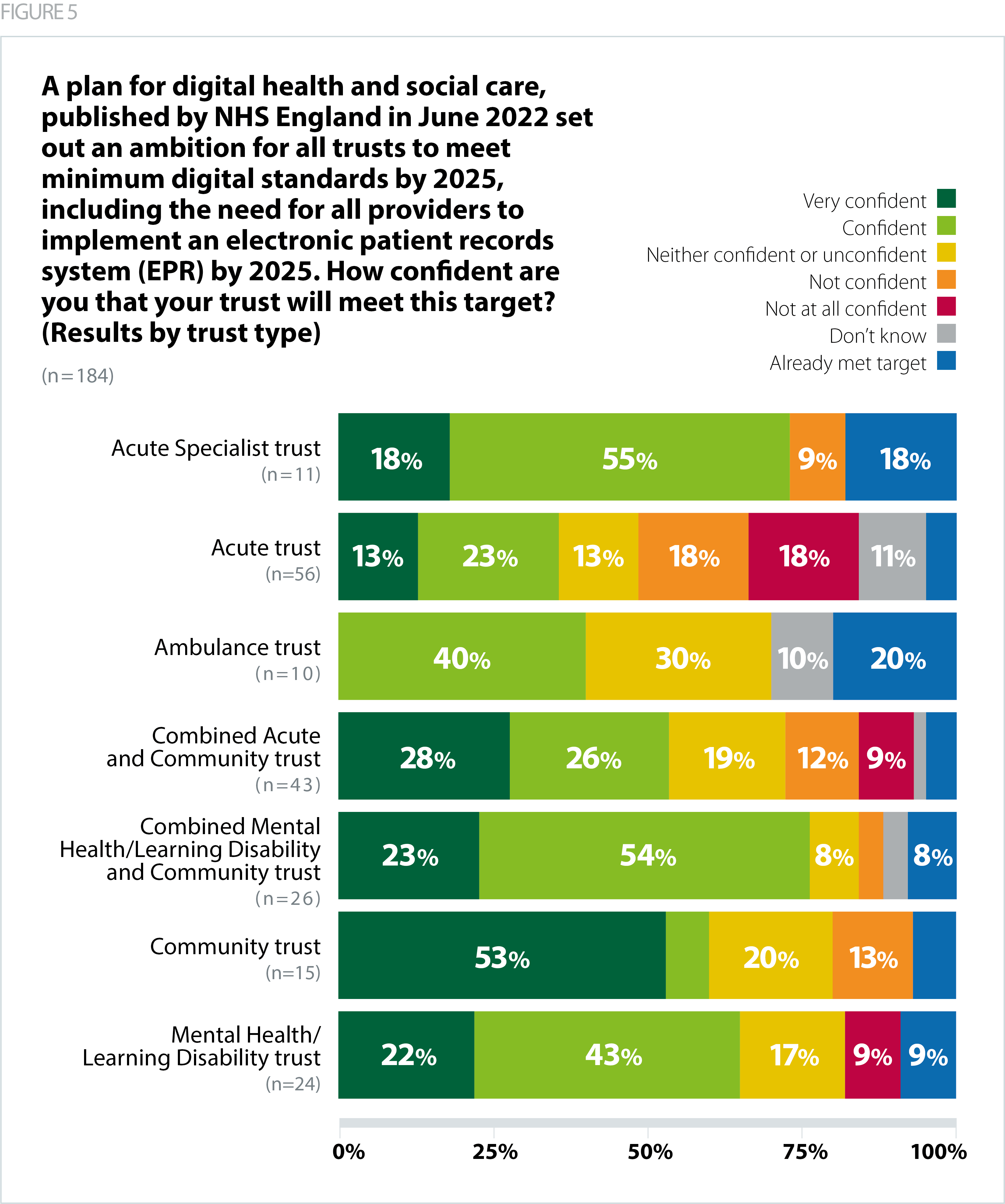
Respondents from combined mental health/ learning disability and community trusts were most likely to say they are very confident or confident that their trust will meet the minimum digital standards by 2025 (23% very confident, 54% confident). This is followed by those from acute specialist trusts whereby 18% said they were very confident and 55% said they were confident. Acute trusts had the lowest confidence levels (18% not confident, 18% not at all confident) compared to other trust types. 20% of ambulance trusts reported they had already met the target, which is the highest among all trust types to date. In the comments, leaders identified challenges with funding as the key reason for not being able to meet the requirements by the date.
What is needed to progress digital transformation
When trust leaders were surveyed on what was needed to make further progress on digital transformation, unsurprisingly the asks were closely linked to many of the barriers that have been highlighted in this report so far.
Sustainable and balanced funding
Trust leaders highlighted the need for a more sustainable long-term funding model that provides reliable access to both capital and revenue funds, and a move away from small pots of funding linked to particular technologies.
We need significant additional funding, both capital and revenue, over multiple years with clear guarantees of the future years' funding.
Making progress requires appropriate levels of funding to enable development - not being constrained by historic funding mechanisms.
An increase in digital skills of workforce and awareness of the need to recruit digital expertise
Respondents said that they require additional, consistent capacity to make further progress on the agenda, and that progress could move faster with a digitally skilled workforce, particularly when large transformation programmes are taking place.
As trusts increase the delivery of health and care services through digital tools, there will need to be an increase in specialists in the workforce who can provide support, particularly with key areas such as AI and cyber. Trust leaders would welcome a longer-term strategic approach to workforce planning through a national DDaT workforce plan.
We need finance and increased skill and capacity in our digital team – it is difficult to recruit skilled staff.
Support and guidance for navigating supplier relationships
The majority of trusts are working with external technology suppliers to deliver their digital programmes. Trust leaders would welcome national assurance and support when managing and navigating supplier relationships. For example national action to hold suppliers to account for delivering interoperability standards.
We have also had serious incidents with software suppliers who have let us down, where poor software quality and support from suppliers has hampered progress.