What is co-production?
Arguably, there has been a lack of agreement on a common definition of co-production, particularly within the health sector. It has often been conflated to encompass a range of different engagement methodologies. Essentially, co-production is a method of engaging with communities, whereby individuals or groups are actively involved in making and shaping decisions related to the delivery of public services.
'Community engagement' is a broader process of working with and involving patients or communities in healthcare services or research. This could include a wide range of participation techniques that seek to elicit the views and experiences of patients, service users or wider community members. By listening to and responding to the voices and experiences of the individuals within a community, decisions taken will be more reflective of community needs and so, potentially more effective. Table 1 summarises some of the various terms and models in relation to community engagement and participation.
Table 1
Figure 1
Spectrum of participation
(People Hub, 2021)
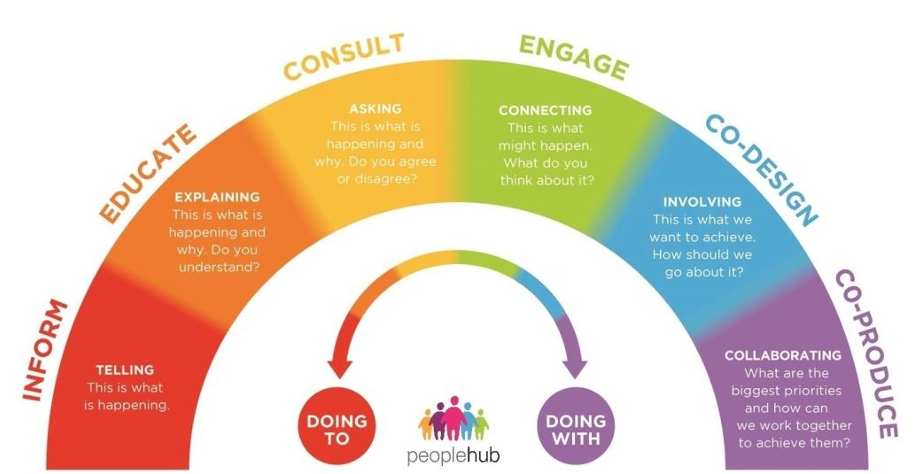
Figure one shows the Spectrum of participation, which highlights the variation in different engagement methods, which each have a distinct purpose that can be effective in different circumstances. Co-production represents a distinct approach that equalises the power dynamic between the organisation seeking information and the individual(s) providing their insights (People Hub, 2021). Co-production is not the same as collaborating with individuals – it involves taking action with communities, to co-create solutions and decisions, with the intended long-term benefit of improving healthcare delivery and outcomes. This represents a more directive shift towards power sharing.
The Care Act (UK Government, 2014) defines co-production as "when you as an individual influence the support and services you receive, or when groups of people get together to influence the way that services are designed, commissioned and delivered".
This may sometimes be referred to as 'collaborative co-production', which emphasises the process of working jointly with individuals and communities at all stages of the engagement process, rather than on an ad-hoc or sporadic basis. In following this method, co-production provides a genuine partnership between organisations and communities. This has often been summarised as "nothing about us without us".
Applying co-production and engagement in healthcare settings
Applying engagement and co-production principles and activities to healthcare settings and services is not new (Realpe & Wallace, 2010). Advocates have long encouraged senior leaders and health professionals alike to engage with their patients to improve the delivery of their care. The Covid-19 pandemic highlighted the value of working in collaboration with communities to implement public health measures and contain transmission among communities (WHO, 2021). Research from the Health Foundation and Public Health Wales (2022) which explored the community-led response to Covid-19, found that drawing on community assets and resources was "instrumental" in responding to the pandemic, particularly in areas with high levels of inequalities. Following the pandemic, co-production and engagement have been increasingly recognised as a useful method for improving services.
NHS England (NHSE)'s guidance Working in partnership with people and communities (NHS England, 2022) sets out principles to enable effective partnership working with communities. The guidance was developed in partnership with NHS Providers, NHS Confederation, the Care Quality Commission (CQC), among others. As statutory guidance that applies to NHS trusts, foundation trusts and integrated care systems (ICSs), it places legal duties on NHS organisations to "involve" the public in their services.
Many trusts are already effectively engaging with their communities to inform their services and the benefits of engaging with communities have been clearly articulated. Later in this report we have included case studies that demonstrate where trusts have applied engagement and co-production methods to target the reduction of health inequalities.
Benefits of engagement with communities in health settings include:
- Improved experiences of care for patients, which is more person-centred and personalised to individual need.
- Empowering patients to better understand their health, connected to improved self-management of treatment and/or conditions. This could potentially prevent the onset of health conditions or the worsening of poor-health.
- Developing trust with individuals and communities, linked to improved access to and engagement with healthcare services and broader preventative initiatives. This could also potentially prevent the onset of health conditions or the worsening of poor-health.
- Improved physical and mental health outcomes for patients, as working in partnership and developing social connections could improve patient recovery (Realpe & Wallace, 2010).
- Improved quality of services and reduced patient safety concerns, potentially resulting in reduced risk of legal challenges.
- Shift within organisational priorities to focus on what matters most to people in their communities, contributing to increased efficiency (McMullin & Needham, 2018).
- Contribution to broader benefits to population health management and the reduction of health inequalities.
- For the individuals involved, there are personal benefits related to the development of skills, confidence, experience of collaboration with professionals and increased peer support.
The New Local have highlighted the benefits of mobilising community assets to prioritise NHS efforts towards prevention, particularly around addressing the wider determinants of health (Lent et al, 2022).