
Introduction
Today, the weekly winter situation reports by NHS England were published, offering once again incredibly valuable insight into the situation on the ground as trusts face a remarkably cold week and prepare for industrial action.
With the ongoing 'twindemic' of COVID-19 and a surge in flu cases and the usual seasonal illnesses, conditions undoubtedly feel challenging. This week's winter data (5 – 11 December) show how bed occupancy remains high with more increases in flu, norovirus and diarrhoea and vomiting (D&V) having an impact on bed capacity. Once again, the data continue to highlight issues with patient flow, with over half of medically fit patients ready for discharge remaining in hospital.
Winter situation report (5 – 11 December)
A&E closures & diverts: There were no A&E closures again this week. There were a total of 15 A&E diverts this week, 11 fewer than the week prior.
Ambulance arrivals: A total of 74,823 patients arrived by ambulance. This is a decrease of about 4% since last week and down by about 11% compared to the same week last year.
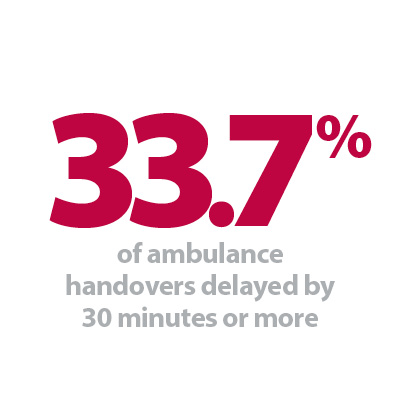
Ambulance handovers: About 34% of ambulance handovers were delayed by 30 minutes or more, up from 31% last week and up from 23% at the same point last year. Nearly 17% were delayed by 60 minutes or more. This is up from 14% last week and up from 10% compared to the same week last year. A total of 29,139 hours were lost to ambulance handover delays.
Critical care: Adult critical care bed occupancy remained at the same level as last week at 80.1%. This is slightly lower than levels seen in the same week last year (80.6%).
D&V: The number of beds closed due to D&V and norovirus has increased this week, with an average of 461 beds closed per day. This is up from 376 last week and also above levels seen this time last year (271).
Discharges: There were an average of 22,343 patients each day who no longer met the criteria to reside, a decrease of about 1%. Of these, 59% (or 13,245) stayed in hospital this week, a similar proportion to last week.
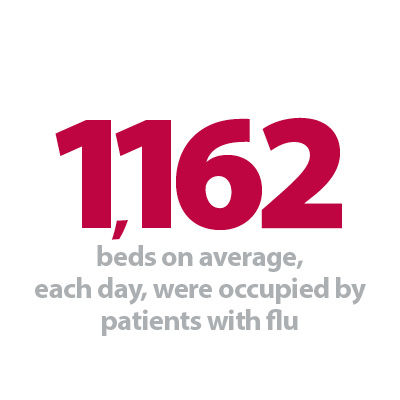
Flu: This week the average number of general and acute (G&A) beds occupied by flu patients each day increased by 63% to 1,162. An average of 87 critical care beds were occupied by flu patients each day this week (45% more than the week before). Compared to the same week last year, the average number of G&A beds occupied by flu patients each day has increased by 4,600% (1,137 more). The average number of critical care beds occupied by flu patients has increased from the same time last year (86 more). These figures are considerably higher compared to this week last year as flu was not as prevalent due to COVID-19 restrictions and social distancing.
G&A beds: There were an average of 99,674 G&A beds open each day – 2,976 more than the same time last year, an increase of about 3%. On average each day 232 beds were unavailable and void due to non-COVID infections. Average bed occupancy remains at 94.5% for the third week in a row. This is an increase of 1.2 percentage points compared to the same week last year.
Long stay: The number of patients staying in hospital longer than seven, 14 and 21 days has increased since last week (up by 0.6%, 1.2% and 0.7% respectively). Compared to the same time last year, the numbers of patients staying in hospital for longer than seven, 14 and 21 days have all increased (up by 12.8%, 19.7%, and 23.9% respectively).
Neonatal intensive care beds: Occupancy has decreased from last week to 69.3%. This is down from 69.7% last week and down from 70.7% the same week a year before. The average number of care beds open is at 1,703, just 0.3% higher than the week before and 1.3% higher than the same week last year.
Paediatric intensive care beds: Occupancy has increased this week to 89.4%, up from 87.8% last week. This is higher than the same week last year (80.8%). The average number of care beds open has fallen slightly to 365 since the previous week (1 fewer care beds open). This is down by 0.8% compared to the same week last year.
Staff absences: There was an average of 56,567 total absences each day this week, of which 11% were COVID-19 related (6,193). The total number of staff absences has once again increased from the week before, but the proportion of COVID-19 related absences has remained similar.
Our view
This week's data show once again cause for concern, with hospitals continuing to face challenging circumstances as temperatures drop.
We continue to see high bed occupancy rates at nearly 95%, with a notable proportion filled with flu patients and COVID-19 patients, all of it impacting the capacity available in hospitals. We are also seeing increases in the number of beds closed due to D&V, and norovirus. Today's figures also show the ongoing issues with patient flow and wider pressures across the health and social care sector, as we see once again that over half of medically fit patients ready for discharge remain in hospital.
As the NHS tackles the impact of seasonal viruses circulating more widely again after social distancing and restrictions, the demand on the urgent care pathway remains high, as seen in the further rise in handover delays, with now over a third being delayed by 30 minutes or more.
Additionally, workforce challenges persist, with staff absences increasing again to over 56,500, which will undoubtedly exacerbate seasonal pressures, all against the backdrop of industrial action.
Association of Ambulance Chief Executives: Ambulance staff 24/7 crisis phoneline
Anna Parry, the deputy managing director at Association of Ambulance Chief Executives (AACE) discusses the new ambulance staff 24/7 crisis phoneline which was designed to meet the mental health needs of ambulance service staff.
On 24 November, an ambulance staff 24/7 crisis phoneline was launched. The provision of this new service has been made possible by funding from NHS England and has been commissioned and co-designed by AACE on behalf of the NHS ambulance sector.
Established in 2011, AACE was created to provide ambulance services with an organisation that can support, co-ordinate and implement nationally agreed policy. It also provides the general public and other stakeholders with a central resource of information about NHS ambulance services.
Ambulance staff have one of the toughest jobs in the country. As well as life's usual stresses and strains, the people in our ambulance services also have to deal with long hours, tough working conditions and emotionally draining call outs. However, it's not only frontline clinicians who can be adversely affected by their job. Increasing demands on our ambulance services are impacting staff members at all levels and in all types of roles.
These pressures can take a toll on the mental health of ambulance service employees, which has been intensified over the last few years by COVID-19; 77% of ambulance staff have said their mental health has got worse since the start of the pandemic.
The ambulance staff charity (TASC) is the national charity dedicated to supporting the mental, physical and financial wellbeing of the UK's ambulance staff. Every year, mental health support is the charity's most in-demand service and accounts for around four in every five interventions they provide.
In just one year, 213 ambulance workers from across a wide range of locations, ages and job roles spoke to TASC about having suicidal thoughts, and one in four of them were actively planning to take their own life.
The ambulance staff 24/7 crisis phoneline has been co-designed by AACE, on behalf of its members, and TASC to meet the mental health needs of ambulance service staff when they are experiencing suicidal ideation or are in crisis. It is also intended to alleviate some of the pressure ambulance service employees can feel when supporting their colleagues by offering a safe, supportive, professional service that can be accessed during both the day and night.
The service includes:
- In-the-moment support to keep people safe and stable. This takes the form of a 24-hour phoneline staffed by qualified counsellors who are experienced in helping people in the blue light services and supported by clinicians.
- Longer-term support once a person is safe and stable, specifically a five-session Collaborative Approach to Managing Suicide support programme, which is tailored for people experiencing suicidal thoughts.
The service is available to all ambulance staff in the UK regardless of their job role or length of service. This service is available to staff in England, Wales, Scotland, Northern Ireland, Isle of Man, Isle of Wight or Guernsey.
Further information on TASC can be found online, as well as additional information about AACE's work to support employee mental health and wellbeing.