
Last week we saw that, on the whole, trusts coped better than expected with demand pressures throughout December. This weeks’ winter sitreps cover the new year and the first week of January - when pressures are notoriously bad. So, how did the first week of 2019 play out in the NHS?
The data points to pressure rising for emergency care and acute services, although the picture remains more positive in several areas compared to last year. Trusts will find it difficult to maintain current performance if factors such as low temperatures, increased flu or norovirus outbreaks hit. A number of key indicators presented a downward trend in the last week:
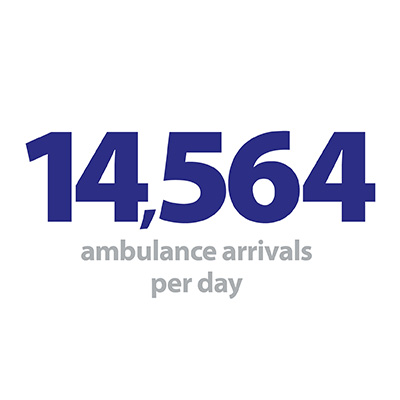
- Ambulance arrivals increased again to a new record high, up 2.8% in the past week to 101,949, or 14,564 arrivals per day.
- Bed occupancy jumped by 5.7% in the past week to 93.2%, with two thirds of trusts running at 95% occupancy or more at some point of the last week.
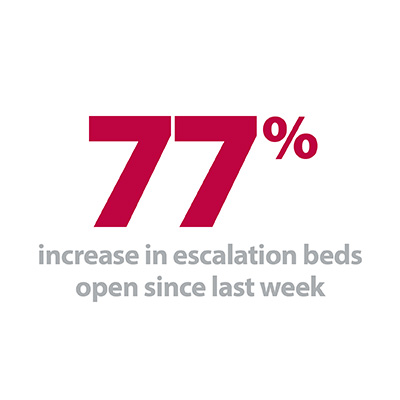
- There were over 1,300 more escalation beds open this week, a rise of 77% as trusts responded to increasing demand.
- Adult critical care bed occupancy rose by 6.5% since last week, another sign that the number of people who are seriously ill is increasing.
- More people are staying longer in hospital, with 8% more people staying for more than 7 days compared to last week, and 10% more staying longer than 21 days.
- Handover delays increased, with 12% of arrivals waiting more than 30 minutes, 2.3% up on last week.
Demand for care is clearly extremely high, and it is perhaps no surprise that maintaining patient flow will be more difficult under the sheer volume that trusts are facing. While ambulance arrivals continue to reach record levels, this only shows the number of ambulances going to hospitals. A significant part of their work includes ‘see and treat’, so this number alone masks the actual activity of ambulance services.
Ambulance arrivals increased again to a new record high, up 2.8% in the past week to 101,949, or 14,564 arrivals per day.
This week saw the highest number of long stay patients this winter for each of the 7, 14 and 21 day cut-offs, and while there may still be some scope to increase the number of escalation beds, this is now also reaching a level not seen since last winter.
The crucial preparatory work of trusts leading into winter, as well as the efforts of staff over the past few weeks mean the system is in a stronger position to respond to the rising demand. Collectively, these figures are not heading in a positive direction, but in comparison to last winter many areas are holding up far better:
- A&E diverts are half what they were at the same point last year.
- D&V and norovirus are having a far smaller impact, with less than half the number of beds currently closed compared with last year.
- While handover delays and long stay patients are higher than the previous week, both are at significantly lower levels than the same point last year.
- Monthly A&E performance data also out this week shows 86.4% of patients were seen within four hours. That is 1.4% better than the same point last year despite 42,500 more attendances and 24,000 more emergency admissions.
The crucial preparatory work of trusts leading into winter, as well as the efforts of staff over the past few weeks mean the system is in a stronger position to respond to the rising demand.
The size of the challenge demonstrated by the rising demand is stark, and trusts deserve credit for the improvements mentioned above. This is a result of better planning, both for winter and in general operations, and better system working with community, primary care, social care and mental health.
As Sam Allen, Chief Executive of Sussex Partnership NHS Foundation Trust, sets out below in her contribution to our winter watch campaign, mental health services are leading the way in driving this system wide focus throughout the year, not just at times of highest demand.
But we must not be complacent. We are hearing from trusts that the pressures have really stepped up over the past few days which we may expect to see reflected in the data next week. Concerns include increases in the number of patients staying over 21 days, more people with severe and complex illness, rising cases of flu, increases in the numbers of people waiting longer than 12 hours and some patients being held in A&E overnight before a bed becomes available.
As we enter the coldest part of the year, trusts will be on edge to maintain current levels of care against the rising demand; with the ability of the system to absorb further pressure set to be tested.
For a more detailed breakdown of this week’s winter sitrep data please see our summary dashboard.
Collaboration is key to making the changes we want to see across health and social care.
This week Sam Allen, chief executive of Sussex Partnership NHS Foundation Trust shares a front line perspective from the mental health sector.
We know winter carries serious risks and places additional demand on NHS and social care services. Providing safe, responsive care is uppermost in the minds of health and social care leaders in the course of our resilience planning.
Like services across the country, we’ve had winter in our sights for some time in order to make sure we’re as prepared as possible. This includes giving 77% of our staff the flu jab, extending a rapid response ambulance triage service, investing in the development of crisis lounges as an alternative to A&E and scoping plans for a 24/7 service for people experiencing a mental health crisis.
Over the past few months we’ve held multi-agency meetings, with the support of our local authorities, and have made good headway on reducing number of people in an acute mental health bed whose discharge is delayed. This needs continued attention, not least in terms of working collaboratively with partners in housing. We have also worked with NHS Improvement and partners to develop a data set for the system to better understand what is happening in relation to mental health presentations in A&E.
Our big challenge is to make sure this degree of system-wide focus exists all year round as a matter of course, not just in anticipation of seasonal spikes in operational pressure (as vital as it undoubtedly is to do this).
Our big challenge is to make sure this degree of system-wide focus exists all year round as a matter of course, not just in anticipation of seasonal spikes in operational pressure (as vital as it undoubtedly is to do this). This is crucial given the sustained demand upon mental health services we’re starting to see all year round. We’re moving in the right direction on this in my local area, and I value the shared commitment to mental health from our partners.
The work we have to do includes determining if we have the right level of capacity, in the right place, in our mental health hospitals as well as our acute hospitals. Bed occupancy across many mental health services runs close to, or at, 100%. This means it can be challenging to arrange timely access to hospital care for people as close as home to possible.
In mental health a significant percentage of urgent acute hospital care activity takes place in the independent sector, not the NHS. This compares to physical health care where the role of the independent sector is mainly restricted to elective care. Imagine attending A&E with appendicitis and needing to be transferred to a hospital up to 200 miles away for your surgery. Whilst we always try hard to avoid the equivalent within mental health services, it does happen. That’s not good for patients or families. Nor is it what staff want for the vulnerable people under our care.
The focus in the NHS Long Term Plan on eliminating out of area placements is welcome and important, as is the commitment to a 24/7 crisis response service for mental health, the development of community services and the importance of meeting the physical and mental health needs of children and young people.
The focus in the NHS Long Term Plan on eliminating out of area placements is welcome and important, as is the commitment to a 24/7 crisis response service for mental health, the development of community services and the importance of meeting the physical and mental health needs of children and young people. It also included a much need emphasis on the need for joined up thinking and care for people with learning disabilities and autism.
As the plan highlights, collaboration is key to making the changes we want to see across health and social care. This involves resisting the almost instinctive, institutional urge that can prompt people to retreat back behind organisational boundaries when the conversations become crunchy or when it’s convenient. I believe there’s a very real understanding that this just isn’t going to cut it any longer given escalating levels of demand, changing population needs and pressure on resources we all face.
We should see these challenges as a spur to be bold, creative and radical in thinking about what kind of health and social care the local communities we serve really need from us. This is a fantastic opportunity, especially if it’s one we choose to take by genuinely working with and listening to others. That includes our partners in the third sector, housing, emergency services (police, ambulance, fire and rescue), as well as the people who use our services and their carers.
There’s no better time for us to push on and really harness the benefits of increased collaboration for the benefit of patients. In the meantime, I want to take this opportunity to acknowledge everyone across health and social care services who works so hard to keep people safe and cared for. It’s what they strive for 365 days a year. They deserve our thanks and appreciation.
Winter pressure building for health and care but preparations by trusts are helping
Responding to the latest weekly winter performance data and combined performance data, the director of policy and strategy at NHS Providers, Miriam Deakin said:
“The latest winter performance data shows that pressure is building for the health and care system as we begin the new year.
“Although performance is better than this time last winter, demand for care is rising steeply – bed occupancy for the week ending 6 January jumped to 93.2% and more patients are arriving at hospital by ambulance than ever before with 102,000 arrivals over the week. Trusts are also telling us that they are increasingly seeing more patients with greater levels of frailty and complex care needs.
“Trusts continue to work flat out to cope with increasing demand. Accident and emergency figures for December show that despite a small but expected dip in performance as we move into the traditional winter months, the preparations that trusts have put into place have helped them go into winter in a stronger position than last year – this is despite an additional 42,000 attendances to A&E and 24,000 emergency admissions than last December. The number of patients forced to wait longer than 12 hours has fallen 46% compared to last year despite the rise in demand. This is a testament to the planning and hard work of trusts and their staff.
We can’t be complacent. Trusts are telling us that the situation on the ground is beginning to heat up with community, mental health and ambulance services all experiencing pressures akin to those working inside hospitals.
“Winter preparations, improvements to the joined up working across health and care and lessons learned from last winter are helping trusts to manage this spike in demand. But we can’t be complacent. Trusts are telling us that the situation on the ground is beginning to heat up with community, mental health and ambulance services all experiencing pressures akin to those working inside hospitals.
“This week the government published its long term plan for the NHS. Its vision to see a shift in care to the community and closer to home will reduce pressure on hospital services. We need to see this plan turn into action, and the overdue social care green paper, to ensure the health and care system can meet these high levels of demand year round.”