When I joined Mersey Care NHS Foundation Trust (MCFT) as chief executive just over seven years ago, I did so without any significant knowledge of the true complexity of mental health presentation, its provision and associated culture. I suppose this gave me the opportunity to ask the seemingly naïve questions that the uninitiated do but which can often be so helpful in providing deep insight. One of the first questions I asked was about the trust’s understanding of those in our care who died by suicide, what had happened, how often and what did we do to learn and close gaps in our processes. Overwhelmingly, people answered these questions with an earnestness and transparency that was encouraging but almost always finished off – and I paraphrase – with the comment ‘…but don’t worry, the trust is way below the national average, not an outlier’.
One of the first questions I asked was about the trust’s understanding of those in our care who died by suicide, what had happened, how often and what did we do to learn and close gaps in our processes.
Chief Executive
Eventually it was the last statement that rang loudest with me, and ultimately our Board, where we collectively saw this as a normalisation of what should, each and every time, be viewed as a catastrophic event. The facts were correct in that MCFT has for many years been in the lowest quintile for suicide rate/10,000 for its patient population. However, when converted to actual lives lost of loved ones while in our service, our Board took the clear view that we needed to radically readjust our individual and corporate mind-set.
Suicide is a truly wicked problem
No easy task. Suicide is a truly complex issue. It is, using the nomenclature of Rittel and Webber, one of the great, persistent wicked problems. Globally more than 800,000 people die by suicide annually, with the figure for England and Wales being 5,370 in 2018. You can do the sums for yourself but the equivalent of something like 13 jumbo jets crashing each year. You can imagine how the public outcry would develop if that was the case!
There is a large and well researched body of evidence on suicide in the UK with about a third of deaths in England and Wales being patients known to mental health services.
Chief Executive
Yet there is a large and well researched body of evidence on suicide in the UK (for example see here) with about a third of deaths in England and Wales being patients known to mental health services. Moreover, Louis Appleby’s team in Manchester have for some years now identified a set of safety issues, which if systematically implemented would lower patient suicide rates. While there has been an improvement over time, there is a concern that there is too much variation in how evidence is put into changed clinical and management practice. Much of the continuous improvement opportunity that is needed to reduce deaths is well described but seems to be slowly adopted and converted into opportunities to save lives. For example, out of area admissions is a risk factor, yet this is an issue which until recently, has received little focused attention.
Changing the paradigm – zero suicide
The MCFT Board has been focused on taking a more radical approach to suicide prevention for our patient cohort and from the start we have seen keeping patients safe from suicide as one of the key pillars of our overall approach to patient safety.
In 2016 we declared our ambition for zero suicide for all patients in our care. At its heart is our belief that a suicide event (attempt or death) is an avoidable outcome in a truly safe healthcare system.
In 2016 we declared our ambition for zero suicide for all patients in our care. At its heart is our belief that a suicide event (attempt or death) is an avoidable outcome in a truly safe healthcare system.
Chief Executive
This approach is simultaneously ambitious, contentious and, for some, confrontational. However, confronted with the question: if the number is not zero, then what is the right number...? For us, it seemed inescapable that our leadership challenge should centre on the elimination of suicide of people in our care. Equally, as we looked at the whole issue of parity between mental and physical health care, we were struck by the difference in ambition by say, post operative mortality improvements and an apparent, if unstated, level of acceptance of the inevitability of death by suicide while in services.
Our declaration of zero suicide has never and never will be a target. Instead we have used it to force our thinking, create breakthrough approaches and to fundamentally and permanently change our cultural attitude to suicidal activity by people in our care. More about the zero suicide movement can be found at Zero Suicide Alliance's (ZSA) website and CIT International.
What have we learnt?
There is not enough space to cover all of the work that has emerged as a result of embracing the ‘power of zero’. But two pieces have been, in my view, disproportionately important and impactful. One has been a simple piece of awareness training, which some of you will recognise as the current ZSA training and the other, the development of a behavioural programme to create psychologically safe spaces for staff to disclose and learn in the event of a patient suicide (or any unintended event for that matter).
The training, originally developed in MCFT as a piece of co-production between those with lived experience and staff, revealed a significant insight: very high percentages of clinical and non-clinical staff considered suicide to be both selfish and inevitable. This poses the simple question of how can we ask people to engage in prevention of suicide if they inherently believe it is inevitable? To what extent have the many iterative prevention programmes been diminished because of this sort of conformation bias?
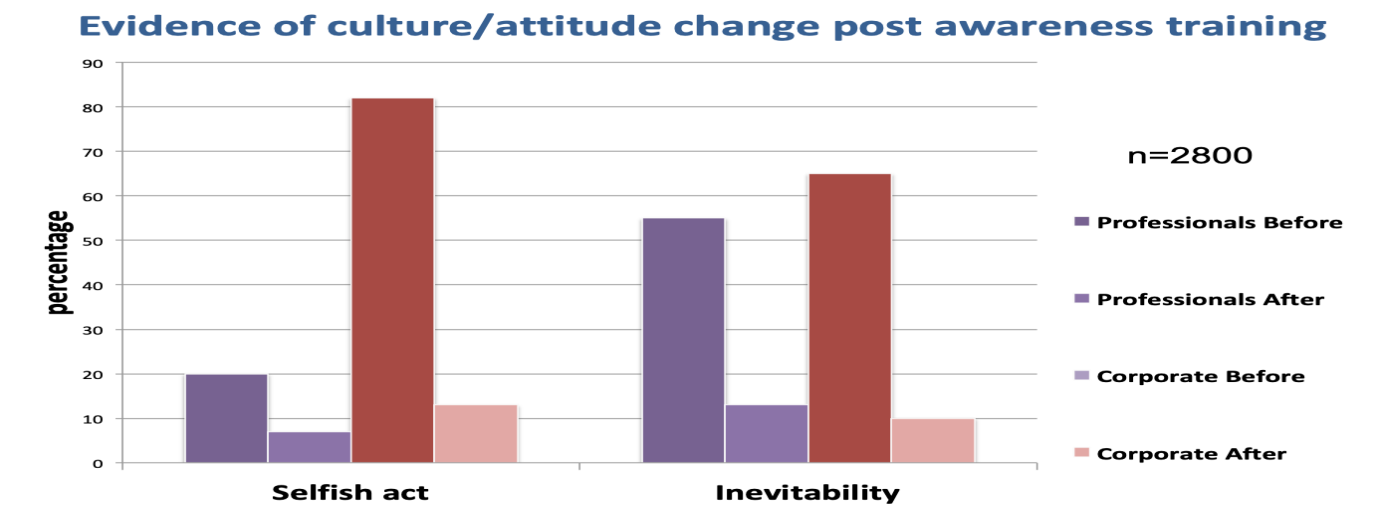
The shift in attitude within 20 to 30 minutes (the time taken to do the training) is frankly profound, with pre-training figures of circa 65 to 70% dropping to about 10%. It is our experience that MCFT staff have become more open to engaging in the whole zero suicide endeavour as a result of the training.
It is our experience that MCFT staff have become more open to engaging in the whole zero suicide endeavour as a result of the training.
Chief Executive
The second significant mind-set challenge for us has been in understanding how to become an organisation that learns from its own practice, particularly in the event of a catastrophic event like a suicide of a person in our care. Again to examine the issues in detail would take more words than are available but the question posed by our staff summed up perfectly the issue: how about zero retribution if you want zero suicide? This challenge gave rise to our Just and Learning Culture programme, with the logic being, simply, if staff do not feel psychologically safe as they debrief after an event, then it is unlikely that full and engaged learning will follow, which may be why some continuous improvement initiatives plateau. For us, increased incident reporting, reduced disciplinary activity and better staff survey figures relating to safer reporting all add to the ingredients necessary for a mature and effective safety platform, without which a zero suicide ambition will wither. You can find more about our Just and Learning work here.
Has all of this had an impact on suicide rates in our care?
The incidence of suicide is complicated to measure because they are rare events and because of the involvement of the coronial system to assign intent. We have been looking at our rolling average rate for the trust for about three years now. The impact of what we have been doing, some of which I touched on in this blog, looks cautiously promising indicating a 25% reduction in rate over the three year period.
What can you do on World Suicide Prevention day 2019 to help?
For those of you in NHS provider organisations reading this today please see suicide prevention as your business. A simple, rapid and free means of supporting everyone to be suicide aware is to join the ZSA and encourage staff to take our training. Remember, if we continue to think suicide is inevitable, then we limit the prevention opportunity.
About the author